May 6, 2023
Cardiovascular Information Systems (CVIS) streamline clinical data management, diagnostics, and treatment for heart-related conditions, enhancing patient care. This article comprehensively defines the term and its semantic relation to Cardiology Information System (CIS.) We also give real-world practical use cases for the systems that cardiologists, cardiac surgeons, and other healthcare professionals rely on to treat patients with heart-related ailments.
What is a Cardiovascular Information System (CVIS)?
In medicine, Cardiovascular Information System (CVIS) and Cardiology Information System (CIS) are interchangeable terms with the same meaning. In this article, we will refer to the term CVIS. A CVIS (or CIS) is a specialized software platform designed to manage, store, and analyze clinical information related to diagnosing, treating, and managing cardiovascular diseases. It is tailored to the needs of cardiologists, cardiac surgeons, and other healthcare professionals involved in caring for patients with heart-related conditions. It can help to improve efficiency by reducing paperwork and automating processes like scheduling and reporting. In addition, a CVIS helps streamline the workflow and improve patient care by integrating various aspects of cardiology practice, including:
Patient Data Management
The system stores and manages patient demographics, medical history, laboratory results, diagnostic images, and treatment plans, enabling easy access and retrieval by healthcare providers. Cardiologists and other healthcare professionals can use patient data management for better patient care by using electronic health records (EHRs) and cardiovascular information systems. These systems help healthcare providers in managing patient data and making informed decisions for diagnosis, treatment, and follow-up care.
Consider the case of cardiac surgery. Before surgery, patients undergo various diagnostic imaging tests, such as echocardiograms, CT scans, and MRIs. A CVIS can capture and store this data, patient history, and vitals. This information can then be used by the cardiac surgeon and care team to help plan the surgery and ensure that the patient receives the most appropriate treatment possible. During surgery, the system can also help monitor the patient’s vital signs and provide real-time updates on any changes in their condition. This allows the care team to adjust their approach as needed and ensure that the patient remains stable throughout the procedure. Following surgery, the system can help manage the patient’s recovery, tracking their progress and any medications or treatments they receive. This data can be used to ensure that the patient is receiving optimal care and that any complications are identified and addressed quickly.
In another example, consider the case of a patient with a history of heart disease who visits the hospital due to chest pain. The patient undergoes various diagnostic tests, such as electrocardiogram (ECG), blood tests, and imaging studies. With the help of a CVIS or EHR, the cardiologist can quickly access the patient’s previous medical records, including history of heart disease, past diagnostic test results, medications, and treatments. This information can help the physician better understand the patient’s condition and identify any potential risk factors for the current symptoms.
The system can consolidate the results of the current diagnostic tests, such as ECG, lab tests, and imaging studies, and display them in an organized manner. This allows the healthcare provider to interpret the results and diagnose accurately. Based on the diagnosis, the cardiologist can create a treatment plan within the system. This plan can be shared with other healthcare professionals involved in the patient’s care, such as the cardiac surgeon or the primary care physician. This collaboration ensures everyone is on the same page regarding the patient’s care, reducing the risk of miscommunication or medical errors.
The patient’s progress can be tracked over time within the system, with regular updates on medications, test results, and any changes to the treatment plan. This allows healthcare providers to evaluate the effectiveness of the treatment and make any necessary adjustments, ensuring optimal patient care. The system can also provide personalized educational materials and resources based on the patient’s condition and treatment plan. This helps the patient understand their condition, adhere to their medication regimen, and actively participate in their care.
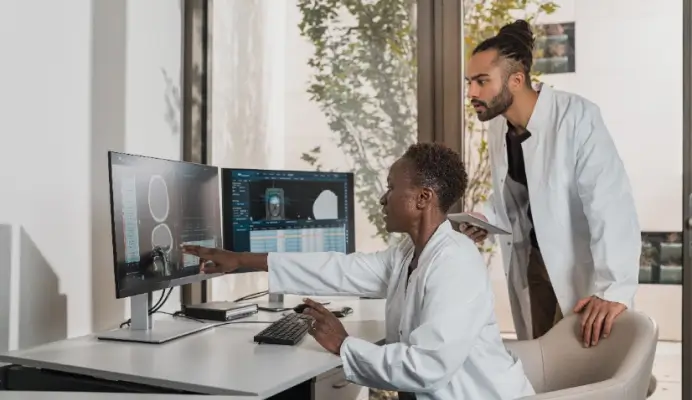
Diagnostic Imaging and Reporting
A CVIS often includes modules for the storage, viewing, and interpretation of diagnostic images. Advanced diagnostic imaging technologies such as computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) can provide highly detailed images of the heart and surrounding tissues.
By using a diagnostic imaging and reporting system, healthcare professionals can quickly and easily access these images and reports, enabling them to make more accurate diagnoses and develop targeted treatment plans. For example, a cardiologist may use a cardiac MRI to identify the location and extent of damage to the heart muscle after a heart attack. They can then use this information to assess the patient’s risk of future events, such as heart failure or arrhythmias, and develop an appropriate treatment plan.
Cardiac surgeons can also use diagnostic imaging and reporting to plan surgical procedures. For example, a cardiac surgeon may use a CT scan to create a three-dimensional model of the patient’s heart and blood vessels prior to performing minimally invasive cardiac surgery. This allows them to accurately map the surgical site, identify potential complications, and plan the optimal approach for the surgery.
In another instance, consider a patient presenting with shortness of breath and chest pain. The patient undergoes an ECG and an echocardiogram to assess their heart function. With the help of a CVIS, the cardiologist can quickly access and review the patient’s ECG and echocardiogram results within the system without the need for physical films or separate viewing platforms. This streamlined access to diagnostic images can expedite the decision-making process and potentially lead to earlier intervention.
The Cardiovascular Information System may offer advanced visualization tools, such as 3D reconstruction or image manipulation, to help the healthcare professional better assess the patient’s heart structure and function. Additionally, some systems may have built-in algorithms or artificial intelligence (AI) capabilities that can aid in interpreting complex imaging studies.
The system can help generate structured reports based on the diagnostic imaging findings, which can be easily shared with other healthcare providers involved in the patient’s care. This standardized format can improve communication between providers and reduce the risk of misinterpretation or missing crucial information.
Furthermore, it can store and organize a patient’s past imaging studies, enabling healthcare professionals to compare the current results with previous findings. This comparison can help identify changes or trends in the patient’s condition and inform appropriate clinical decisions. This fosters multi-disciplinary team collaboration, as different subspecialties can efficiently collaborate using the diagnostic imaging and reporting features of the system. For example, a cardiac surgeon may review an angiogram to determine the need for coronary artery bypass surgery, while a cardiologist can use the same information to plan for medical management or percutaneous coronary intervention.
Clinical Decision Support
Some CVIS systems have built-in algorithms and tools that assist healthcare providers in making evidence-based decisions regarding diagnosing and treating cardiovascular conditions. For example, consider the management of patients with heart failure. Heart failure is a complex condition requiring multiple medications, frequent monitoring, and a range of treatments tailored to each patient’s specific needs.
A Clinical Decision Support (CDS) system can help guide healthcare professionals through the complex decision-making process of managing heart failure. For instance, it can provide alerts when a patient’s vital signs, laboratory tests, or medications fall outside safe or optimal ranges. It can also provide decision support to help healthcare professionals choose the most appropriate medications or treatments for each patient based on their clinical history, medication history, and other relevant factors.
Consider a patient with chest pain suspected of having coronary artery disease (CAD) in another use case. The cardiologist needs to determine the most appropriate diagnostic test and treatment strategy for this patient. The system may have built-in tools to calculate the patient’s risk of CAD based on factors such as age, gender, medical history, and clinical presentation. This risk assessment can help the healthcare provider determine the most appropriate diagnostic tests and interventions for the patient.
Based on the patient’s risk stratification, the clinical decision support system may suggest appropriate diagnostic tests, such as stress testing, coronary computed tomography angiography (CCTA), or cardiac catheterization. By following evidence-based recommendations, healthcare providers can minimize the risk of unnecessary or invasive testing and focus on the most effective diagnostic approaches.
Once the diagnosis has been confirmed, the CDS can provide evidence-based treatment recommendations tailored to the patient’s specific condition and risk profile. These recommendations may include lifestyle modifications, medications, or interventional procedures. The system can also help the healthcare provider determine the optimal timing and sequence of these interventions to maximize patient outcomes.
Furthermore, it can alert healthcare providers to potential drug interactions or contraindications based on the patient’s medication history and comorbidities. This information can help prevent adverse events and ensure the patient receives the most appropriate and safe treatment. Lastly, it can help healthcare providers track the patient’s progress, adjust treatment plans as needed, and schedule regular follow-up appointments to monitor their condition. The system can also generate alerts or reminders for essential milestones, such as medication titration or follow-up testing.
Workflow Management
The CVIS can help organize and streamline the workflow in cardiology departments by automating tasks such as appointment scheduling, billing, and communication between healthcare providers.
For example, managing a patient who has undergone a cardiac catheterization. Several healthcare professionals may need to be involved in the care and treatment of the patient, including the cardiologist who performed the procedure, the nursing staff, and the interventional radiologist who may need to review the images.
A Workflow Management system can help coordinate patient care by facilitating communication and actions among the various healthcare professionals involved in the process. For instance, it can automatically notify the nursing staff when the patient is ready to be transferred to the recovery area, alert the interventional radiologist when the images are ready for review, and notify the cardiologist of any changes in the patient’s vital signs or condition.
Integration with other Health Information Systems
A comprehensive CVIS can interface with other hospital or clinic systems, such as electronic health records (EHRs), laboratory information systems (LIS), and radiology information systems (RIS), to facilitate seamless data exchange and collaboration among healthcare providers.
For instance, a patient with heart failure may also have comorbidities such as diabetes or chronic obstructive pulmonary disease (COPD). By integrating the patient’s electronic health record (EHR) with other health information systems, such as the diabetes management system or pulmonary function testing software, healthcare professionals can have a more comprehensive view of the patient’s health status and treatment history.
This information can be used to develop a more targeted and effective treatment plan for the patient, considering their unique medical history, risk factors, and comorbidities. It also helps healthcare professionals identify potential drug interactions and ensure that patients receive the most appropriate medications for their condition.
Research and Quality Improvement
CVIS systems can be used to collect and analyze data for research purposes and to track performance metrics and outcomes for continuous quality improvement in the delivery of cardiovascular care.
Healthcare professionals can use data analytics tools to analyze clinical data captured in the CVIS to identify patterns and trends in patient outcomes and treatment effectiveness. This can help identify areas for improvement in care delivery and ultimately lead to better patient outcomes.
For example, a cardiologist may use data from a CVIS to analyze the outcomes of patients who received a certain type of cardiac intervention, such as coronary artery bypass surgery. By comparing results between patients who received the intervention and those who did not, the cardiologist can identify factors that may improve outcomes, such as patient selection criteria or changes in surgical technique. The system can also identify variations in practice patterns between healthcare providers, which can help identify more effective treatment protocols and reduce variability in care delivery.
By centralizing and organizing cardiology-related information, a CVIS helps enhance the efficiency and quality of patient care, promotes data-driven decision-making, and supports research and quality improvement efforts in the field of cardiovascular medicine. Take advantage of the opportunity to revolutionize your cardiology practice and enhance patient care with Intelerad’s Cardiovascular System Solutions. Request a demo today and discover how our comprehensive CVIS solution can streamline your workflow, improve clinical decision-making, and foster better collaboration among your healthcare team. Experience firsthand the transformative impact of our CVIS on your facility’s efficiency and patient outcomes.